- OBJECTIVE:
To lay down a procedure for the management of the clinical supplies of pharmaceutical products.
- SCOPE:
This standard operating procedure is applicable for formulation plant. Management of Clinical Supplies shall involve the following:
- Procurement of reference drug.
- Unpacking and repacking of reference drug.
- Manufacturing and packing of batches of test drug/ investigational product (IP) for clinical trials.
- Dispatch of clinical trial supply to CRO.
- Recall and destruction procedures of IP.
- RESPONSIBILITY:
- Head, Clinical Research or his/her designee shall be responsible for elucidating the number of reference drug/ comparator required for carrying the clinical trials and then conveying the same to Materials Management for the procurement of the same.
- Head, Materials Management or his/her designee shall be responsible for procurement of reference drugs and providing related documents to Stores.
- Head, Stores or his/her designee shall be responsible for storage and issuance of materials for converting the same into clinical supplies by Production.
- Head, Production or his/her designee shall be responsible for manufacturing, unpacking, re-packing of the materials for clinical trials.
- Head, QC or his/ her designee shall be responsible for verification of the reference drug and testing of the clinical trial batches
- Head, R&D or his/her designee and Head, QA or his/her designee shall be responsible for proving the necessary documents for manufacturing, unpacking, re-packing of the materials for clinical trials.
- Head, QA or his/her designee shall be responsible for release of the clinical trial batches and compliance of this SOP.
Click the link to download word file copy of this document: https://pharmaguidehub.com/product/management-of-clinical-supplies-in-pharmaceutical/
- DEFINITIONS:
Reference Drug: Drug which shall be used as comparator in the clinical trials on test drug.
- Clinical trials are a type of research that studies new tests and treatments and evaluates their effects on human health outcomes. People volunteer to take part in clinical trials to test medical interventions including drugs, cells, and other biological products, surgical procedures, radiological procedures, devices, behavioral treatments, and preventive care.
- Clinical trials are carefully designed, reviewed, and completed, and need to be approved before they can start. People of all ages can take part in clinical trials, including children.
- There are 4 phases of biomedical clinical trials:
Phase I studies usually test new drugs for the first time in a small group of people to evaluate a safe dosage range and identify side effects.
Phase II studies test treatments that have been found to be safe in Phase I but now need a larger group of human subjects to monitor for any adverse effects.
Phase III studies are conducted on larger populations and in different regions and countries, and are often the step right before a new treatment is approved.
Phase IV studies take place after country approval and there is a need for further testing in a wide population over a longer timeframe.
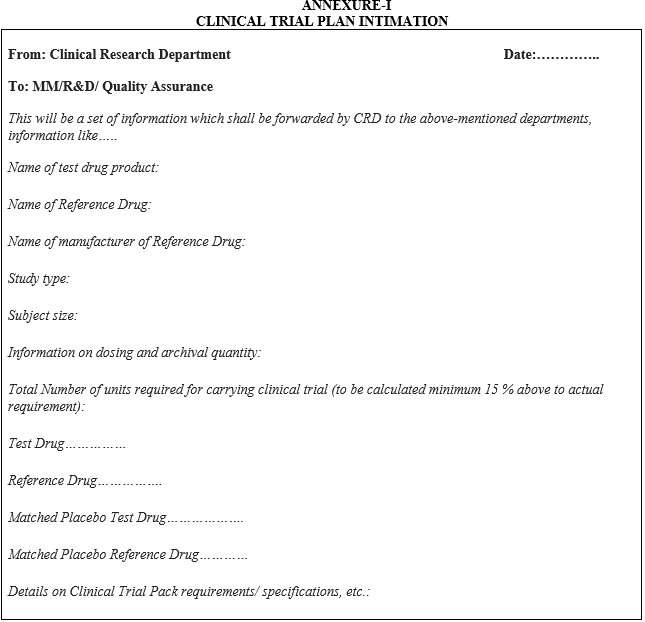
- Clinical research shall submit the plan for conduct of clinical trials to Quality Assurance, R&D and Materials Management by furnishing information as indicated in Annexure-1.
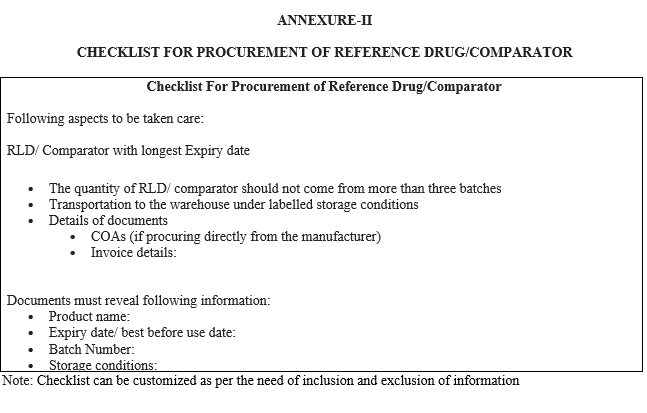
- Materials Management shall procure the reference drug as per Annexure-2 (Checklist) and shall forward the reference drug to manufacturing site.
- Stores at manufacturing site shall store the reference drug in the designated area under the labeled storage conditions and copy of relevant documents (like invoice copy, etc.) received with the supply shall be forwarded to QA.
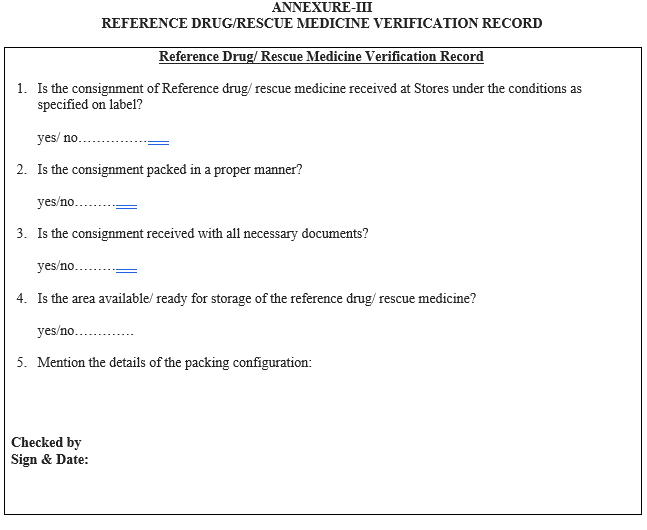
- QA shall perform the physical verification as per the checklist as described in Annexure-3 and shall submit the sample(s) to QC for testing, if desired by Head-QA.
- Necessary documentation like manufacturing and packaging TDs, Specifications and Standard Test Procedures for In-process and finished goods testing required for clinical trial batches shall be taken care collectively by R&D and QA.
- R&D shall prepare manufacturing and packaging TDs for clinical match placebos and packaging TDs for reference drug and QA shall review and approve the documents for final implementation.
- QA shall prepare a protocol-cum-report for carrying issuance, unpacking, packing, dispatch (to CRO) of the reference and test drug products in clinical trial packs.
- The protocol for unpacking and packing of reference drug shall include information, but not limited to, responsibility chart, storage of reference drug, issuance procedure, unpacking procedure, storage procedure of unpacked units, labeling information at various stages, reconciliation procedures of medicine and labels, blinding procedures (if required), destruction procedures of labels and medicine, flow chart indicating the process of flow, etc.
Click the link to download word file copy of this document: https://pharmaguidehub.com/product/management-of-clinical-supplies-in-pharmaceutical/
- QA shall assess the pre-requisites (availability of documents/ procedures and facility/area) before planning the manufacturing of batches for clinical trials.
- QA shall issue the BMR to Production for manufacturing of clinical trial batches.
- The Batch Number to clinical match placebo and test drug shall be assigned.
- The reference drug shall be unpacked and then shall be repacked in the intended packs for clinical trials and shall bear the original batch number(s) (assigned by its manufacturer).
- The manufacturing date and expiry date in the manufacturing records and labels on the final packs to be taken up for blinding activity (if undertaken in-house) before sending to CRO of test product and related clinical placebos shall be as per SOP.
- The production on clinical supplies shall be planned in such a way that there should be no parallel production of drug product and clinical match placebos.
- IPQA shall give line clearance before the commencement of activity at production floor.
- The reference drug shall be unpacked in the area under controlled environmental conditions.
- In case, the test drug if already packed [in case from Exhibit batch(s)] shall be re-packed for clinical trials as per the methodology adopted for reference drug i.e. using protocol prepared by QA.
- The primary pack shall contain information in reference to Annexure-4.
- After completion of packing operations, the sample shall be collected by IPQA and sent to QC for analysis. IPQA shall fix labels on the packs with product related information before sending to QC for testing.
- QC shall analyze the samples as per respective Standard Test Procedures. QC shall issue certificate of analysis.
- Randomization/ blinding of the IP shall be undertaken by Designated Person as per the procedures laid down by Clinical Research Department.
- The clinical trial supplies shall be put on stability studies for minimum one year as per ICH guidelines at QC of the manufacturing site to know so that the products should be within the pre-established specification throughout the trial duration.
- A sufficient quantity of final packs shall be retained as retention sample by QA.
- QA shall release the clinical trial batches for blinding and repacking, if required, for clinical studies. The release shall be done through a certificate carrying remarks on conformance of the product with established specifications and revelation of manufacturing under cGMP standards. Certificate shall carry the remarks ‘For Clinical Trial Use Only’.
- Upon release of CT batches by QA, in case of blinding done in-house finally DP shall release the batches after review all the relevant document.
- The packing for dispatch to respective CRO shall be done and related information shall be captured in the format as described in Annexure-5 (Clinical Supply- Dispatch Record)
- The clinical supplies shall be transported through a pre-qualified courier under the desired storage conditions. The courier details shall be filed in the respective BMR/ Protocol.
- Copy of dispatch details shall be sent to the concerned Medical Monitor from Clinical Research Department by QA.
- The warehousing and inventory of the IP at CRO shall be monitored by Medical Monitor.
- Destruction procedures for IP shall be prepared by QA, and shall be given to CRO if agreed to be destroyed at CRO site.
- In case of recall, the recall process shall be facilitated by Medical Monitor from unit side. The IP shall be received at manufacturing site, reconciled and destroyed.
- Returned IP (recalled) shall be accounted and destroyed by QA.
- QA shall maintain complete reconciliation record of the investigational materials.
- Movement record of the IP from the warehouse of CRO to different investigational sites shall be in access of unit. to account the reconciliation of IP.
- Details of supply of rescue medication(s) shall be addressed in the product specific protocol. The rescue medication shall be labeled with ‘For Clinical Trial Use Only’ statement.
- In case of Clinical Trial Supply to Regulatory markets, Qualified Person shall release the clinical trial samples for dispatch to CRO based on the understanding from facility audit, analytical results of the supply samples, report of handling of clinical trial supply and compliance statement of Designated Person.
Click the link to download word file copy of this document: https://pharmaguidehub.com/product/management-of-clinical-supplies-in-pharmaceutical/
- REFERENCES:
Not Applicable
- ANNEXURES:
| ANNEXURE No. | TITLE OF ANNEXURE |
| Annexure-I | Clinical Trial Plan Intimation |
| Annexure-II | Checklist for Procurement of Reference Drug/Comparator |
| Annexure-III | Reference Drug/Rescue Medicine Verification Record |
| Annexure-IV | Labeling Information for Clinical Trials |
| Annexure-V | Clinical Supply- Dispatch Record |
- DISTRIBUTION:
| Control copy No. 1 | : | Head Quality Assurance |
| Control copy No. 2 | : | Head Quality Control |
| Control copy No. 3 | : | Head Production |
| Control copy No. 4 | : | Head Purchase |
| Control Copy No.5 | : | Head Warehouse |
| Control Copy No.6 | : | Clinical Research |
| Control Copy No.7 | Research and Development | |
| Control Copy No.8 | Regulatory Affairs | |
| Master Copy | : | Quality Assurance Department |
- ABBREVIATIONS:
| RLD | : | Reference Listed Drug |
| COA | : | Certificate of Analysis |
| IP | : | Materials Management |
| MM | : | Active Pharmaceutical Ingradients |
| RH | : | Relative humidity |
| CRO | : | Contract Research Organization, who shall carry clinical trials |
| TDs | : | Technical Directions |
| DP | : | Designated Person |
| QP | : | Qualified Person |
| CRD | : | Clinical Research Department |
| R&D | : | Research and Development |
| IPQA | : | In process Quality Assurance |
- REVISION HISTORY:
CHANGE HISTORY LOG
| Revision No. | Details of Changes | Reason for Change | Effective Date |
| 00 | New SOP | Not Applicable | To be written manual |
ANNEXURE-I
CLINICAL TRIAL PLAN INTIMATION
ANNEXURE-II
CHECKLIST FOR PROCUREMENT OF REFERENCE DRUG/COMPARATOR
ANNEXURE-III
REFERENCE DRUG/RESCUE MEDICINE VERIFICATION RECORD
ANNEXURE-IV
LABELING INFORMATION FOR CLINICAL TRIALS

ANNEXURE-V
CLINICAL SUPPLY- DISPATCH RECORD

Click the link to download word file copy of this document: https://pharmaguidehub.com/product/management-of-clinical-supplies-in-pharmaceutical/
Frequently Asked Questions?
Frequently Asked Questions on Management of Clinical Supplies in Pharmaceutical
1. What are clinical supplies?
Clinical supplies refer to any drug, device, biological product, or other investigational product used in a clinical trial. They can include active ingredients, placebos, comparator drugs, medical devices, and labels.
2. Why is effective management of clinical supplies important?
Effective management of clinical supplies is crucial for ensuring:
- Patient safety: Accurate dispensing and tracking of supplies minimizes the risk of medication errors and adverse events.
- Trial integrity: Maintaining proper controls over supplies guarantees data integrity and regulatory compliance.
- Cost efficiency: Managing inventory and minimizing wastage reduces unnecessary expenses.
- Trial timelines: Timely availability of supplies prevents delays in patient recruitment and trial completion.
3. What are the key elements of effective clinical supply management?
- Accurate forecasting and budgeting: Predicting supply needs for the entire trial duration ensures sufficient availability and avoids overstocking.
- Robust procurement and sourcing: Identifying reliable suppliers and negotiating optimal prices with proper quality control protocols.
- Secure storage and distribution: Implementing temperature-controlled facilities, secure storage practices, and trackable distribution channels.
- Inventory management: Utilizing inventory management systems to monitor stock levels, prevent stockouts, and optimize batch management.
- Compliance with regulations: Ensuring adherence to Good Manufacturing Practices (GMP), Good Clinical Practice (GCP), and relevant regional regulations.
- Risk management: Proactive identification and mitigation of potential supply chain risks, such as delays, shortages, or temperature excursions.
4. What are some common challenges in managing clinical supplies?
- Complex logistics: Managing diverse supply chains with intricate temperature requirements and international transportation.
- Changing trial protocol: Adapting supply needs to protocol amendments or unforeseen patient enrollment trends.
- Global regulations: Navigating different regulatory requirements across trial locations.
- Counterfeiting and diversion: Implementing anti-counterfeiting measures and ensuring secure distribution channels.
- Technology integration: Utilizing appropriate software and tracking systems to manage data and automate processes.
5. What are some emerging trends in clinical supply management?
- Decentralized trials: Managing supplies for geographically dispersed patients and clinical sites.
- Direct-to-patient shipping: Securely delivering supplies directly to patients at home.
- Real-time monitoring: Utilizing sensors and tracking systems for real-time supply visibility and improved control.
- Big data analytics: Leveraging data from various sources to optimize forecasting, improve risk management, and predict stockouts.
6. Where can I find more information on clinical supply management?
- Regulatory agencies (FDA, EMA, etc.)
- Industry associations (PhRMA, DIA, etc.)
- Clinical research organizations (CROs)
- Supply chain management consultants
- Online resources and training courses
Click the link to download word file copy of this document: https://pharmaguidehub.com/product/management-of-clinical-supplies-in-pharmaceutical/